
Ditstek Innovations developed a comprehensive cloud-based health insurance claims management system tailored for TPAs, insurers, and Medicare Advantage plans. The platform replaces legacy AS/400 infrastructures with a robust, real-time solution that enables rapid payer onboarding, automated claims adjudication, integrated billing, and 24/7 data visibility. Built with modern microservices and secure cloud infrastructure, the system seamlessly connects with clearinghouses, banking systems, and provider portals. It enhances healthcare claims processing software workflows while ensuring scalability, compliance, and interoperability across payer networks. This digital transformation drastically reduces manual dependencies, improves client retention, and empowers back-office operations with live analytics and mobile-first member engagement.

New payer partners faced a 14–16 month delay before system go-live, significantly stalling revenue streams and limiting competitiveness in a rapidly evolving healthcare landscape.

Batch processing left staff in the dark, unable to access live claims or eligibility data—compromising decisions, member service quality, and time-sensitive claim approvals.

Key departments operated on isolated workflows. Enrollment, EDI, billing, and mailroom processing tools lacked a shared interface—leading to inefficiencies and redundant manual tasks.

Finance and executive teams compiled reports manually from spreadsheets, consuming days of work and leaving no room for agile decision-making or real-time operational monitoring.

The aging AS/400 infrastructure struggled under high-volume member updates and EDI traffic, limiting the organization's ability to scale and meet peak-time processing demands.
Our platform empowered real-time claims administration through scalable infrastructure, automation, API integration, and embedded analytics—streamlining workflows and future-proofing operations.

Built on modern architecture, the system ensures real-time visibility into member updates, claims, and premiums across devices and APIs—enhancing healthcare claims automation accuracy and response speed.

Integrated connectors allow seamless data flow between clearinghouses, banks, and portals, making the platform a powerful TPA claims management software engine for high-volume claims data exchange.

Users gain access to real-time KPIs via intuitive dashboards and a no-code report builder, eliminating the need for Excel-based compilation across the claims administration software suite.

A pre-built vendor integration kit and sandbox environment helped reduce onboarding timelines from over a year to just 3–4 months—accelerating revenue generation and client activation.

Our rule-based claims adjudication software handles medical, vision, dental, and disability claims, integrating with bank reconciliation systems to reduce manual validations and approval cycles.

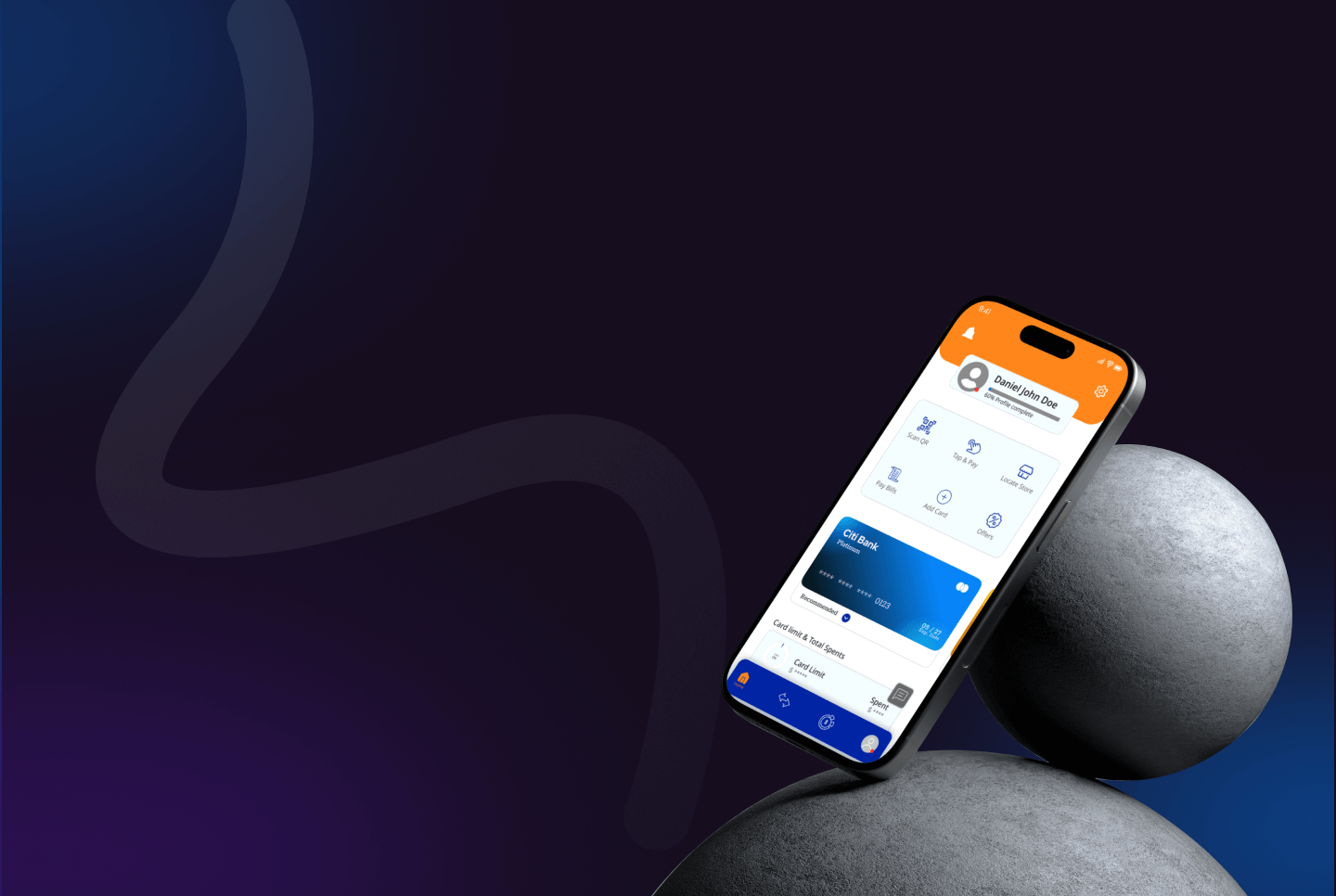
GDPR-ready apps support two-factor authentication, interactive ID cards, and multi-locale, multi-currency setups—offering members secure access to plan details and claim statuses.

Claims, invoicing, KPI reports, fee schedule imports, and ID card printing were unified into a modular platform for optimized billing and healthcare claims processing software operations.

Supports multi-frequency premium schedules and intuitive plan comparison tools, offering members flexibility and transparency while streamlining back-office premium reconciliation.

Real-time dashboards provide full audit trails for 835/837 and custom payer files, enhancing compliance, visibility, and faster eligibility checks across all payers.

Members can register, recover credentials, view claims, and receive premium alerts via mobile—driving higher engagement and reducing customer service dependency.

Includes scanning, mailroom automation, and vendor onboarding tools—digitizing traditionally paper-heavy workflows and reducing manual overhead for administrators and processing teams.
By replacing outdated processes with a plug-and-play onboarding kit, payer go-live timelines dropped from 14–16 months to just 3–4 months, boosting early-stage ROI.
Payers stayed engaged through transparent operations and powerful self-service tools that minimized back-and-forth and accelerated issue resolution.
Batch-based reporting cycles were replaced with real-time dashboards, cutting decision lag from days to seconds and enabling proactive intervention.
The event-driven system architecture allows frictionless scaling during open enrollment and high-traffic periods without latency or performance degradation.
Automated reconciliations and dashboard-driven insights helped teams avoid manual data merges—freeing dozens of hours every month for strategic work.
Secure, scalable healthcare practice management software for allied health clinics, streamlining scheduling, billing, and patient care.
Discover trusted medical treatment abroad with our medical tourism platform, offering secure bookings, consultations, and global care coordination.
Streamlined behavioral health billing with cloud-based RCM software, AI-driven claims management, and real-time insurance integration.
Cloud-based EMR and behavioral health EHR with patient engagement software, HIPAA compliant portal, and secure healthcare analytics for better care delivery.
HIPAA-compliant SaaS healthcare platform unifying IoT in healthcare, RPM, and automated reporting for chronic disease and public-health programs.
HIPAA-compliant telehealth physical therapy platform with remote patient monitoring, guided rehab, and analytics to improve MSK recovery outcomes.
Scalable wellness app development with appointment scheduling API, secure user authentication, and health metrics dashboard for measurable outcomes.
Explore remote patient monitoring software for chronic care, behavioral health, and transitional care compliant, scalable, and patient-focused.
HIPAA-compliant AI telehealth app with computer vision for MSK care, real-time motion tracking, pain mapping, and remote patient monitoring.
AI-powered mental wellness app with 24/7 emotional support, mood tracking, habit coaching, and secure analytics for scalable mental health care.
Streamline care delivery with healthcare management software integrating medical billing, workforce tracking, and revenue cycle automation.
A scalable cloud-based SaaS platform designed to modernize healthcare claims automation for TPAs, insurers, and Medicare Advantage providers with real-time processing, onboarding accelerators, and advanced analytics.
HIPAA-compliant behavioral health EHR software streamlining clinical, billing, and intake workflows for mental health, recovery, and human services providers.
HIPAA-compliant on-demand marketplace for therapy with real-time scheduling, secure profiles, and scalable open-source software for therapists.
A scalable cloud-based claims administration platform for TPAs, insurers, and Medicare providers—streamlining onboarding, processing, and analytics.
Custom cloud-based fitness app with virtual coaching, workout tracking, nutrition plans, and goal-driven features for trainers, users, and admins.
We built a secure, scalable telehealth app with remote patient monitoring for Australian healthcare—delivering virtual consultations, billing, and compliance.
Eco-friendly affiliate marketing software enabling carbon-neutral shopping, coupon savings, and real-time carbon emission tracking at scale.
Discover a cloud-based POS and retail ERP system unifying HR, inventory, ticketing, and training—built for multi-store retail business efficiency.
Scalable SaaS gift registry platform for nonprofits, delivering charity gifting software solutions with secure payments and rural development impact.
Boost florist sales with our SaaS eCommerce platform for B2B & B2C. POS, CRM, and mobile tools streamline operations and enhance customer retention.
Cloud-based tanning salon software with POS, booking, automation, and analytics to streamline operations and boost customer retention.
Cloud-based CRE marketing software with online real estate BOV module, MLS integration, and marketing automation for faster property deals.
Streamline rentals with tenant management software, AI in property management, and proptech software development for smarter real estate operations.
Discover our scalable virtual learning platform development with real-time classes, session management dashboard, and learning management system services.
Custom online lesson planner and eLearning platform for K–12 & higher ed—curated content, student tagging, and reusable templates for impactful teaching.
Modular academic advising software and degree planning tool with ERP integration, secure role-based access, and real-time course scheduling.

AI-powered online education platform with interactive eTextbooks, adaptive assessments, and real-time analytics to boost engagement and readiness.
Automotive lending software automating dealer loan workflows with real-time integrations, fee validation, and instant approvals for faster financing.
Automated B2B invoicing software with recurring billing, real-time tracking, and Azure serverless architecture for secure, scalable operations.
End-to-end digital lending platform with BNPL, auto lease software, and Arabic localization, built by a leading fintech software development company.
Scalable fintech app for currency exchange, forex cards, and remittances—delivering automation, compliance, and real-time global transactions.
Custom fintech app unifying 100+ services into a B2B/B2C fintech solution with real-time visibility and automated workflows.
Enterprise platform for automated trade data ingestion. Multi vendor marketplace development and service marketplace app development with Snowflake & Salesforce.
Secure cross border payment platform with digital wallet app, invoicing, subscriptions, and ML-based fraud detection for global businesses.
Discover a SaaS fintech platform on Azure that streamlines loan management, lender integration, and financing workflows, delivering instant approvals and enhanced customer experience.
Auto claims management software with parts procurement, BI analytics, and workflow automation to streamline insurance repairs and supplier collaboration.
Automated rental management system with online rental booking software to boost efficiency, bookings, and customer experience for rental businesses.
Custom AI face recognition software with biometric security, legal takedowns, and verified access to safeguard digital privacy and identity.
Built a real-time payment analytics platform for the Govt aided platforms with workflow automation solutions and multilingual workflow automation capabilities.
Enterprise SaaS for automated billing with RBAC implementation and single sign-on integration, boosting accuracy, governance, and global finance workflows.
Cloud-based tanning salon software with POS, booking, automation, and analytics to streamline operations and boost customer retention.
Azure-hosted court case management software enabling secure workflows, real-time data sync, and streamlined inter-agency coordination.
Real-time whale sightings app and whale alert system using advanced marine conservation technology for ocean wildlife protection and tracking.
All-in-one employee engagement platform uniting communication, learning, and recognition to boost productivity and collaboration in modern workplaces.
A creative scorebook collaboration platform with real-time notation, event integration, and multi-device access—built for musicians, educators, and ensembles.
A centralized SaaS platform for motorcycle and powersports dealers—streamlining sales, financing, insurance, and trade-ins for faster deal closures.
Scalable B2B travel portal development integrating flights, hotels & tours with real-time booking. Built for global travel software companies.
Secure business workflow automation software integrating offender case management, financial account handling, and digital process automation services.
Discover RoadSight, a custom-built travel assistance software and an AI-powered, voice-first travel and tourism app for safer, smarter, hands-free exploration.
SaaS-based event ticketing software development with secure seat selection, Stripe payments, and real-time check-ins for modern online event management.
A secure, mobile-first offender management platform designed for pre-release and community corrections, enabling real-time tracking, secure communication, and treatment plan access to improve compliance, transparency, and rehabilitation outcomes across correctional facilities.
We developed a construction safety management platform with real-time risk tracking, gamification, and offline access for high-risk industries.
AI-driven legal document automation software with clause libraries, logic management, and CLM integration—boosting accuracy, compliance, and speed.
Cloud-based SaaS asset management software with real-time alerts, predictive analytics, and reporting to replace manual tracking and boost efficiency.
A secure, mobile-first offender case management platform with GPS tracking, secure messaging, and automation to boost compliance and transparency.
ASAM-based addiction management software for treatment centers. Streamline substance abuse treatment with structured care plans and integrated billing.
Discover how our SMS automation software and referral marketing platform helped small businesses boost acquisition, loyalty, and ROI.
End-to-end truck repair management software with automation, digital vehicle inspections, and multi-branch scalability for auto repair businesses.
Responsible sourcing software with ESG compliance tools, human rights due diligence, and supply chain transparency to improve worker engagement.
Modernize urban mobility with our smart parking management system. Explore intelligent parking solutions for cities to streamline tracking, payments & enforcement.
Scalable custom SaaS platform with AI advisor matching, enterprise CRM tools, and high-speed search for global expert consultations.
Streamline care delivery with healthcare management software integrating medical billing, workforce tracking, and revenue cycle automation.
Eco-friendly affiliate marketing software enabling carbon-neutral shopping, coupon savings, and real-time carbon emission tracking at scale.
Cloud-based CRE marketing software with online real estate BOV module, MLS integration, and marketing automation for faster property deals.
Enterprise platform for automated trade data ingestion. Multi vendor marketplace development and service marketplace app development with Snowflake & Salesforce.
Streamlined behavioral health billing with cloud-based RCM software, AI-driven claims management, and real-time insurance integration.
Streamline rentals with tenant management software, AI in property management, and proptech software development for smarter real estate operations.
Cloud-based EMR and behavioral health EHR with patient engagement software, HIPAA compliant portal, and secure healthcare analytics for better care delivery.
Scalable wellness app development with appointment scheduling API, secure user authentication, and health metrics dashboard for measurable outcomes.

AI-powered smart farm monitoring system with ammonia sensor barn tracking, real-time alerts, and predictive insights for safer, compliant operations.
Discover a SaaS fintech platform on Azure that streamlines loan management, lender integration, and financing workflows, delivering instant approvals and enhanced customer experience.
Discover a cloud-based POS and retail ERP system unifying HR, inventory, ticketing, and training—built for multi-store retail business efficiency.
Cloud-based tour booking platform with AI-driven tools for fishing charters, hiking tours, and guides. Secure payments, scalability, and growth-ready SaaS.
.png)
Cyclist-first marketplace with events, bike-friendly lodging, and gear shops—built with Laravel for scalable vacation rental app development services.
A secure, scalable Peer to Peer Rental Marketplace enabling local item sharing, reducing waste, and empowering communities to monetize idle assets with safe, intuitive rental workflows and smart transaction controls.
Scalable UGC marketplace app with escrow, FedEx, licensing & analytics—built by an expert marketplace app development company for secure brand-creator campaigns.
Discover crowdfunding app development with donation matching, SaaS dashboards, and recurring memberships for nonprofits and crowdfunded.
A smart parking solutions with real-time search, booking, and payments. Scalable parking management system for drivers, hosts, and admins.
Automated rental management system with online rental booking software to boost efficiency, bookings, and customer experience for rental businesses.
Discover our scalable virtual learning platform development with real-time classes, session management dashboard, and learning management system services.
Enterprise platform for automated trade data ingestion. Multi vendor marketplace development and service marketplace app development with Snowflake & Salesforce.
Custom cloud-based fitness app with virtual coaching, workout tracking, nutrition plans, and goal-driven features for trainers, users, and admins.
Cloud-based tour booking platform with AI-driven tools for fishing charters, hiking tours, and guides. Secure payments, scalability, and growth-ready SaaS.
Digital customs document clearance software for freight forwarders with real-time tracking, automation, and compliance-ready solutions.
IoT-based energy monitoring system using smart power quality analytics for real-time tracking, cost savings, and sustainability in facilities.
Smart IoT lighting and HVAC control system with QR code access control and real-time energy management for efficient building operations.
Enterprise SaaS IoT asset tracking software for security operations with real-time monitoring, incident reporting, and mobile-ready dashboards.
Modernize urban mobility with our smart parking management system. Explore intelligent parking solutions for cities to streamline tracking, payments & enforcement.
IoT-driven smart greenhouse automation with climate control, soil moisture sensors, and Hortimod OS for precision agriculture and higher yields.

AI-powered smart farm monitoring system with ammonia sensor barn tracking, real-time alerts, and predictive insights for safer, compliant operations.
Cloud-native IoT tracking system with GPS, video intelligence, and remote device control for scalable, future-ready asset management across industries.

Discover IoT-based smart water management system development services for real-time monitoring, supply control, and scalable smart city solutions.
Explore remote patient monitoring software for chronic care, behavioral health, and transitional care compliant, scalable, and patient-focused.
HIPAA-compliant SaaS healthcare platform unifying IoT in healthcare, RPM, and automated reporting for chronic disease and public-health programs.
Automotive lending software automating dealer loan workflows with real-time integrations, fee validation, and instant approvals for faster financing.
We developed a construction safety management platform with real-time risk tracking, gamification, and offline access for high-risk industries.
IoT-based energy monitoring system using smart power quality analytics for real-time tracking, cost savings, and sustainability in facilities.
Smart IoT lighting and HVAC control system with QR code access control and real-time energy management for efficient building operations.

Discover IoT-based smart water management system development services for real-time monitoring, supply control, and scalable smart city solutions.
End-to-end truck repair management software with automation, digital vehicle inspections, and multi-branch scalability for auto repair businesses.
Built a real-time payment analytics platform for the Govt aided platforms with workflow automation solutions and multilingual workflow automation capabilities.
Cloud-based tanning salon software with POS, booking, automation, and analytics to streamline operations and boost customer retention.
ASAM-based addiction management software for treatment centers. Streamline substance abuse treatment with structured care plans and integrated billing.
Azure-hosted court case management software enabling secure workflows, real-time data sync, and streamlined inter-agency coordination.
A secure, mobile-first offender case management platform with GPS tracking, secure messaging, and automation to boost compliance and transparency.
Automotive lending software automating dealer loan workflows with real-time integrations, fee validation, and instant approvals for faster financing.
AI-driven legal document automation software with clause libraries, logic management, and CLM integration—boosting accuracy, compliance, and speed.
We developed a construction safety management platform with real-time risk tracking, gamification, and offline access for high-risk industries.
Discover a cloud-based POS and retail ERP system unifying HR, inventory, ticketing, and training—built for multi-store retail business efficiency.
SaaS-based event ticketing software development with secure seat selection, Stripe payments, and real-time check-ins for modern online event management.
Discover how our SMS automation software and referral marketing platform helped small businesses boost acquisition, loyalty, and ROI.
Explore remote patient monitoring software for chronic care, behavioral health, and transitional care compliant, scalable, and patient-focused.
Automated rental management system with online rental booking software to boost efficiency, bookings, and customer experience for rental businesses.
Boost florist sales with our SaaS eCommerce platform for B2B & B2C. POS, CRM, and mobile tools streamline operations and enhance customer retention.
Custom fintech app unifying 100+ services into a B2B/B2C fintech solution with real-time visibility and automated workflows.
Enterprise SaaS for automated billing with RBAC implementation and single sign-on integration, boosting accuracy, governance, and global finance workflows.
Streamline rentals with tenant management software, AI in property management, and proptech software development for smarter real estate operations.
Scalable wellness app development with appointment scheduling API, secure user authentication, and health metrics dashboard for measurable outcomes.
Custom cloud-based fitness app with virtual coaching, workout tracking, nutrition plans, and goal-driven features for trainers, users, and admins.
Scalable UGC marketplace app with escrow, FedEx, licensing & analytics—built by an expert marketplace app development company for secure brand-creator campaigns.
HIPAA-compliant AI telehealth app with computer vision for MSK care, real-time motion tracking, pain mapping, and remote patient monitoring.
IoT-driven smart greenhouse automation with climate control, soil moisture sensors, and Hortimod OS for precision agriculture and higher yields.
Secure business workflow automation software integrating offender case management, financial account handling, and digital process automation services.
Cloud-based CRE marketing software with online real estate BOV module, MLS integration, and marketing automation for faster property deals.
ASAM-based addiction management software for treatment centers. Streamline substance abuse treatment with structured care plans and integrated billing.
Azure-hosted court case management software enabling secure workflows, real-time data sync, and streamlined inter-agency coordination.

AI-powered smart farm monitoring system with ammonia sensor barn tracking, real-time alerts, and predictive insights for safer, compliant operations.
Discover a SaaS fintech platform on Azure that streamlines loan management, lender integration, and financing workflows, delivering instant approvals and enhanced customer experience.
Discover a cloud-based POS and retail ERP system unifying HR, inventory, ticketing, and training—built for multi-store retail business efficiency.
Discover how our tailored SaaS solutions can modernize your claims processing, onboarding, and analytics for smarter payer operations.
Get a Free Consultation