Healthcare Data Integration: Benefits, Challenges, and Real-Time Solutions
Table Of Content
Published Date :
08 Jul 2025
In today’s rapidly evolving healthcare industry, data is everywhere, but it is often trapped in numerous systems that do not share information with each other. Between EHRs, lab results, insurance claims, patient portals, and other systems, crucial information is often siloed, limiting its impact on care delivery and operational efficiency.
Healthcare data integration provides a solution to this issue by enabling disconnected data sources to be unified in a single view and to engage in real-time capabilities.
In this blog, we will explore how integration achieves clinical outcomes, improves workflows, and addresses challenges such as interoperability, data quality, and compliance. Regardless of whether you are a provider, administrator, or IT leader, it is essential to understand integration to deliver future-proof healthcare.
Healthcare Data Integration Market
The healthcare data integration market is expanding due to the worldwide adoption of electronic health record (EHR) systems by healthcare organizations. As of 2025, the value of the healthcare data integration market is USD 23.48 billion, and it's expected to grow to USD 43.66 billion by 2034. These stats reflect a compound annual growth of 7.13 CAGR for the forecast period.
What is Data Integration in Healthcare?
A healthcare organization's ability to deliver better care depends on its ability to access and interpret patient data effectively when needed. However, in reality, this data is often scattered across disparate systems, including EHRs, insurance platforms, pharmacy databases, and patient portals. These silos create serious roadblocks to operational efficiency and decision-making.
Healthcare data integration solutions break down these silos and bring together data from multiple sources into a single, unified view. This allows organizations to see the complete picture of patient histories, treatments, medications, and more, which helps medical staff in making informed decisions.
Beyond simply combining data, data integration facilitates the cleaning, organizing, and standardization of healthcare data. This enables the production of reliable, high-quality data that is structured and ready for use in management's decision-making. Healthcare staff use this data for decision-making at various stages of patient treatment. Ultimately, meaningful insights enable healthcare providers to deliver a higher quality of service.
Break Down Data Barriers Across Your Healthcare Ecosystem!
DITS connects your scattered systems into one seamless data network; because healthcare decisions shouldn't wait on fragmented records.
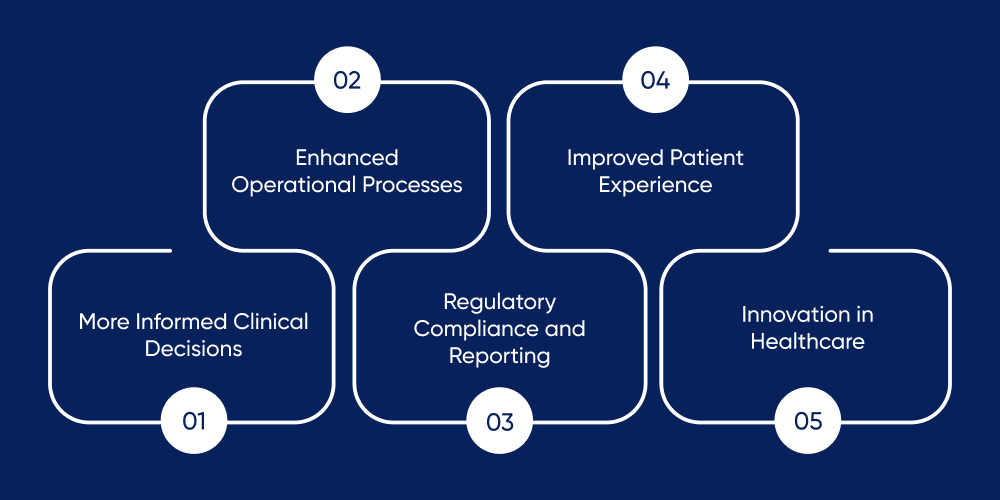
Why is Data Integration Important in Healthcare
The healthcare field uses one of the largest types of data but also one of the most fragmented. Patient data is often stored in silos across the healthcare domain, including hospitals, clinics, separate labs and imaging centers, insurers, and personal devices (why are people without health data from those devices)? When it is not combined and reusable, the data creates a liability that could have been an asset.
1. More Informed Clinical Decisions
For providers and care teams to make the best decisions regarding patient care, they must have access to a complete and accurate record of the patient's medical history. If lab results, specialists’ reports, imaging systems, and wearables are integrated in real-time, providers can:
- See potential issues sooner
- Eliminate duplicate testing
- Utilize evidence-based care
Visualize the potential of diagnostics if a cardiologist could access a patient’s recent ECG, blood work, and wearable heart rate data simultaneously, without any questions, and without needing to search for information.
2. Enhanced Operational Processes
Hospitals and clinics employed numerous manual and non-digitized processes, consuming a significant amount of their staff's time by requiring them to manually enter patient information multiple times, or blaming the fax machine for information loss between departments. Integrated data systems are capable of:
- Reducing patient intake and discharge times
- Automating workflows (appointment reminders, insurance pre-auth)
- Reducing errors from duplicate or transcribed data
That one extra layer of efficiency adds up to more time and productivity on the provider side, that reduces administrative burdens and expenses across any healthcare system.
3. Regulatory Compliance and Reporting
Healthcare providers are facing a growing number of regulatory requirements by CMS, HIPAA and various regulatory agencies. Data integration helps you to:
- Audit access to PHI and make audit trails.
- Compile reports, including those required by government programs like value-based care or quality measures.
- Ensure that privacy and security standards are upheld at every point of data access and use.
4. Improved Patient Experience
When it comes to patients, integrated systems give them:
- A single health record that they can access via a patient portal or their mobile app.
- More timely responses from providers, since their systems are all in sync internally.
- More seamless care coordination across all providers of care, including primary care, specialists, and even behavioral health.
This produces higher patient satisfaction, better patient adherence, and improved patient outcomes.
5. Innovation in Healthcare
When organizations achieve unified datasets, they can:
- Develop artificial intelligence and machine learning models for predictive medicine to enable earlier diagnoses.
- Accelerate the scaling of clinical research and drug trials more quickly than before.
- Review population health data trends to implement preventative measures on even broader scales.
In other words, shortly after initial healthcare integration, let the next "big" innovation begin, and allow evidence-based medicine to guide the route to smarter, more predictive, personalized care!
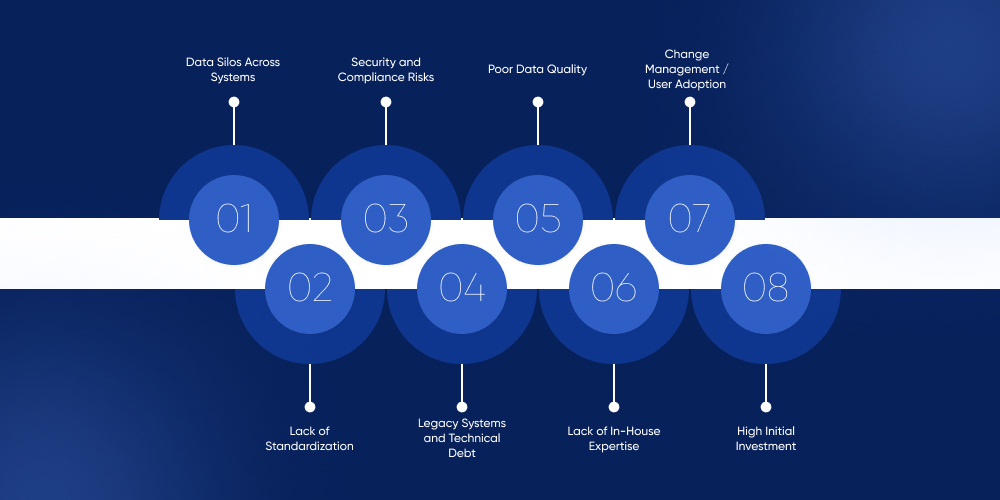
Healthcare Data Integration Challenges
The benefits of healthcare data integration services do not come without challenges. Here are some challenges that healthcare organizations must overcome to implement data integration successfully.
1. Data Silos Across Systems
Healthcare data is information that typically resides in various social systems, including EHRs, lab software, billing platforms, and insurance databases. Very few of these systems are designed to communicate with each other; thus, integration is often complex and expensive.
Impact: Disconnected workflows, redundant data entry, and incomplete patient records.
2. Lack of Standardization
Different systems use various data formats, data structures, and communication protocols. In the absence of standardization (such as HL7 or FHIR), merging data from sources of distinct origin could lead to misunderstandings or the loss of critical information.
Impact: Data that is inconsistent or inaccurate, more technical overhead, and ultimately failed integrations.
3. Security and Compliance Risks
Healthcare data is highly sensitive and heavily regulated. Any integration must be done in compliance with laws such as HIPAA, GDPR, or local data privacy legislation. Increasing the number of connected systems also increases the risk of breaches or non-compliance.
Impact: Legal fallbacks, reputational damage, and loss of patient trust.
4. Legacy Systems and Technical Debt
Many healthcare organizations utilize legacy systems that do not accommodate the use of modern integration protocols. These outdated systems often take time and resources to replace or upgrade; unfortunately, healthcare organizations generally do not have dedicated time or resources to do this.
Impact: High implementation costs and extended timelines.
5. Poor Data Quality
Long-after systems have been integrated into the organization, poor-quality data characterized by things such as duplicated, incomplete, and outdated records may have a detrimental effect. The near future generally requires clean data to make actionable insights.
Impact: Erroneous clinical decisions and reduced faith in data generated by integrated systems.
6. Lack of In-House Expertise
Not all healthcare organizations will have in-house expertise to design and manage a data integration strategy. The result is reliance on vendor partners and increased complexity of implementations.
Impact: Delays, overruns, and suboptimal solutions.
7. Change Management / User Adoption
Some level of new technology, such as the implementation of a new integrated system may cause some professionals to change or interrupt workflows that are ingrained over time. Equipment and expertise will not solve bad workflows that may persist without appropriate training, steering, or change management.
Impact: Low user adoption, increased frustration, and poor ROI.
8. High Initial Investment
Although any data integration solution not only has long-term value but also generally has very high initial costs. Small and mid-sized providers struggle somewhat to understand the full investment of an infrastructure software, data integration, security expertise, and so on.
Impact: Budget constraints may limit all involvement.
Turn Complex Data Challenges into Seamless Healthcare Solutions!
From interoperability issues to legacy systems, DITS helps you tackle integration roadblocks with smart, secure, and scalable strategies tailored to your needs.
Overcoming Data Integration Challenges with DITS
When it comes to healthcare data integration, we at DITS recognize that it is much more than merely connecting systems. We work with you to break down your data silos, enhance data quality, promote compliance, and modernize your infrastructure with a custom strategy tailored to your workflows.
Our experts collaborate with healthcare organizations to enable secure, scalable, future-ready integrations that drive real outcomes, improving everything from operational efficiencies to better patient care.
Best Practices for Successful Healthcare Data Integration

Healthcare data integration is more than just linking systems; it includes developing a standardized and scalable base that is safe, secure, and clinically relevant. To help you carry out integrations successfully and sustainably, here are some best practices to implement:
Identify Your Data Before You Integrate
Identify each data source that you rely on for productivity—EHRs, lab systems, payer platforms, and patient portals, for example. Keep track of where the data resides, how it flows, and which systems depend on it. Once you have a clear outline of your data environment, you can create a structured and efficient integration environment.
Build for Scale Day 1
Healthcare operational environments are constantly evolving, and your integration strategy should adapt accordingly. Invest in flexible, cloud-based solutions that enable you to create a dynamic integration architecture. The only option is scalability to future-proof your projects.
Build with standards, such as FHIR
Standards such as FHIR provide a way to securely and cohesively exchange data between systems that are otherwise incapable of data exchange. You can think of it as your systems employing as standard language so that the sharing, knowing, and doing from patient data is seamless without ambiguity and errors in translation.
Value Data Quality at Every Opportunity
There is nothing worse than introducing unreliable data, which can create even bigger problems with data quality. Utilize automated validation and cleansing tools, work in cycles to analyze and audit data, and continually familiarize yourself with the origin and collection methods of your data. Clean data piles lead to clean insights, reduce the amount of clinical error, and support better decision-making quality at every level of operation.
Develop a Robust Security Framework
Healthcare data is a prime target for exploitation. Encryption, multi-factor authentication, and security reviews should be considered on the same level as healthcare system integrations, built into the integration strategy rather than bolted on. Robust security provisions will help reduce risk and enable better compliance with regulations such as HIPAA, while maintaining patient trust.
Create Structured Data Governance
The actual integration piece is just as critical to implementing a successful integration framework as developing the pieces that lead to the ultimate product. It is not just about technology; the organization or function of your data is equally important. Define roles regarding ownership of data and access from both a control and stewardship perspective. A well-defined data governance framework will maintain the temporal reliability, accountability, and stewardship of that data, making it available to the right people at the right time and the right level of access.
Secure, Real-Time Healthcare Integration with DITS
At DITS, we have a dedicated software development team specializing in building healthcare solutions for organizations seeking operational efficiency, cost optimization, and compliance adherence. Our team works to integrate healthcare data, minimizing data silos and improving coordination between your systems.
Our experienced development team works closely with your business to better understand your requirements and offer a comprehensive data integration solution that is secure, scalable, and future-ready.
We have healthcare clients worldwide, boasting a successful track record and a 97% client retention rate. With a decade of experience in custom software development, DITS is the company you can trust for healthcare data integration services and software solutions.
Are you ready to streamline your healthcare data? Visit our website or click on any button in this post to fill in some details, and we will get back to you shortly.
Need Help With Data Integration? Let DITS Handle the Complexity!
From scalable integration architectures to security and interoperability, DITS delivers tailored solutions that make your healthcare data work harder and smarter.
Conclusion
Healthcare data integration enables efficient, coordinated, and patient-centered care. Integration can support healthcare organizations in making quicker decisions, reducing costs, and improving outcomes by breaking down data silos, enhancing data quality, and delivering relevant information as the patient journey unfolds.
Although challenges such as interoperability, data security, and system complexity persist, the right strategy and technology partner can typically turn these challenges into opportunities. To lead in a rapidly evolving healthcare landscape, organizations must embrace data integration within their healthcare facilities.
FAQs
1. What is data integration in healthcare?
Data integration in healthcare combines data from multiple sources, such as EHRs, lab systems, imaging applications, and patient billing applications, into a single source of truth. This allows healthcare providers to view a patient's full medical history in one place, supporting better clinical decision-making and coordination across departments, enabling greater operational efficiency.
2. Why is data integration important in healthcare?
Healthcare data integration solutions are essential to ensure real-time clinical decision-making, accurate reporting, timely care, and coordination that reflects each patient's full medical history. Integrated data allows for better population management reporting and analytics reduced duplication of services, all of which lead to better patient outcomes and operational efficiencies.
3. What are healthcare data integration standards?
Healthcare data integration occurs through standards including HL7, FHIR, CDA, and DICOM ensuring data is exchanged across applications securely and consistently. These standards allow different healthcare applications to interconnect, enabling interoperability.
4. What are the challenges faced during data integration?
There are difficulties surrounding healthcare data integration services such as incompatible data formats, inconsistent data quality challenges, legacy systems, and regulatory compliance. Security, privacy (e.g. HIPAA), and mapping data across different platforms is difficult. It takes significant technical know-how, a strong commitment to invest in tools and technology, and following industry protocols and procedures to solve this issue.
5. Is Ditstek Flow HIPAA-compliant?
Absolutely. Ditstek Flow is completely HIPAA-compliant. The platform supports strong data encryption, secure access, and regular auditing procedures to protect sensitive health information (PHI). Additionally, the platform is built to ensure every data exchange and data storage process is compliant with the strict privacy and security requirements required by the HIPAA regulations.
6. Can Ditstek integrate with legacy healthcare systems?
Yes! Ditstek has integrated with many legacy healthcare systems. It uses custom APIs, middleware, and standards such as HL7 and FHIR to facilitate seamless interoperability between modern applications and legacy healthcare infrastructures, thus preserving the valuable data while digitally transforming without a full system replacement.

Nidhi Thakur
With more than 19 years of experience - I represent a team of professionals that specializes in the healthcare and business and workflow automation domains. The team consists of experienced full-stack developers supported by senior system analysts who have developed multiple bespoke applications for Healthcare, Business Automation, Retail, IOT, Ed-tech domains for startups and Enterprise Level clients.
Recent Posts

From basic monitoring to enterprise-wide control, energy management system costs depend on your needs. Here’s what influences pricing.

The cost to develop a Transportation Management System (TMS) varies widely, from basic apps at $4,000 - $40,000 for an MVP, to complex, enterprise-level platforms costing $100,000 - $800,000+.

Looking for a Fuel Management System in South Africa? DITS delivers smart, secure fuel monitoring solutions to reduce theft, track usage, and cut costs.

 Doha Exhibition and Convention Center (DECC)
Doha Exhibition and Convention Center (DECC)