Why do you need Healthcare Claim Management Software
Table Of Content
Published Date :
22 Jan 2025
Healthcare claims management is a big deal for both healthcare providers and patients. The process takes a health insurance claim from the initial submission of details to the final payment. And when it works smoothly, everyone benefits.
But when it doesn’t? Well, that’s where things get tricky.
Ever tried processing a healthcare claim manually?
The never-ending paperwork, the back-and-forth with insurers, and the frustration of constant denials is enough to make anyone want to throw in the towel. But what if there was a way to make the entire process smoother, faster, and far less stressful?
Lucky for you, there is!
With healthcare claim management software—your key to transforming how claims are processed and drastically improving efficiency. What is it? How does it benefit you? Hold your horses; we’re here with all the answers you need!
In this blog, we’ll dive into the common challenges that make manual claim management such a headache, explore how healthcare claim management software can revolutionize the process, and guide you on selecting the best solution for your needs.
We’ll also show you how DITS can help streamline your claims management and enhance customer satisfaction. Ready to say goodbye to the old, tedious process? Let’s dive in!
Challenges in Manual Healthcare Claim Management
Despite the numerous benefits of health insurance claims for service providers, insurers and end users, there are various challenges that need to be addressed. A health insurance claim is a complex and time-consuming process, especially when done manually. Let’s understand some significant and common challenges in healthcare claim management.
Complexities in Processing of Claims
The minor details involved in the processing of health claims, including the verification, validation, and final calculation of payout, make the process complex and lead to delays in processing and customer dissatisfaction.
Regulatory Compliance
Adhering to the regulatory compliance and guidelines of health insurance, along with implementing precise measures to prevent and detect false claims, adds more complexity to the process.
High Administrative Costs
The high administrative costs act as a major challenge in the processing of healthcare claims. Private healthcare plans in the United States spend $158 billion in administrative expenses annually. The paper-based process, multiple touchpoints, human intervention, and high cost of reprocessing contribute to athe dministrative costs of healthcare systems.
High Rate of Denials
The high rate of denials due to the ineligibility of users and incomplete or incorrect user information contributes to the high rate of denials in healthcare claims. A high rate of denials further leads to unnecessary waste of time and resources.
Data Security
The manual handling of tasks and paperwork involved in the process leads to insecurity of customer data. The loss of user data can lead to a high rate of denials or delays in claims processing. Also, data insecurity contributes to non-compliance with industry standards and regulations.
Say Goodbye To Claim Errors, Delays, & Denials With DITS!
Experience seamless claims management with software built to simplify workflows and improve financial outcomes.
The Transformative Role of Software in Healthcare Claims Management
Now that you know what’s broken in the system, let’s talk about how to fix it! The use of insurance claim management software can make the processes run more smoothly and efficiently. By automating routine tasks, you’ll witness faster processing of claims, allowing healthcare providers to save time and focus on core tasks and issues that demand attention.
Plus, software lets you cross-verify names, addresses, calculations, and final payouts within seconds while improving compliance and customer satisfaction due to fast processing and high data accuracy. Let’s understand the benefits in detail:
Benefits of Healthcare Claim Management Software
Faster Processing Times
Automating the claim process significantly speeds up everything from verification to final settlement, reducing delays and getting results to patients and providers more quickly.
Improved Accuracy
By minimizing human errors, healthcare claim management tools ensure that data is entered correctly, helping to prevent costly mistakes that could lead to denials or delays.
Reduced Denials and Rework
Automated checks for eligibility, document verification, and compliance rules can help identify issues early, preventing denials and the need for rework.
Better Compliance
Healthcare claim management software is designed to keep you aligned with ever-changing industry regulations and standards, ensuring that your claims meet all necessary compliance requirements.
Enhanced Transparency
Real-time tracking and reporting provide clear visibility into each step of the claim process, improving communication between providers, insurers, and patients, and making it easier to resolve issues quickly.
Must-Have Features of Healthcare Claims Management Software
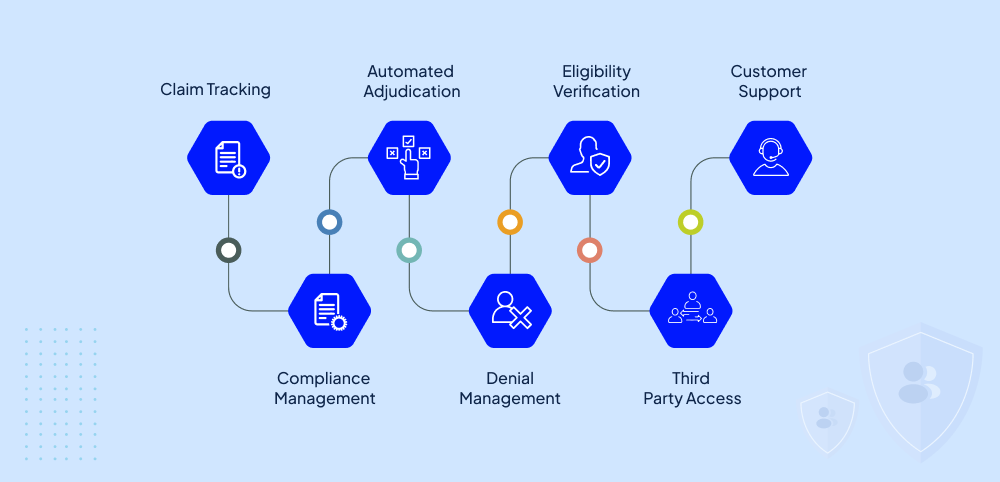
You must be wondering why we keep going on and on about why this is such a crucial software, but now let’s strengthen your understanding by delving into what precisely such solutions should have so that you can actually reap the long list of benefits that you just skimmed through! Here are the key features that every user should look for before choosing a healthcare claims management tool.
1. Claim Tracking
Claim tracking is an essential part of any claim management application. The real time tracking adds transparency to the process and improves the operational efficiency while minimizing errors and optimizing performance. The tracking feature also allows insurers and healthcare providers to monitor the progress of claims at any stage of the process.
2. Compliance Management
Compliance management refers to the processes that service providers and insurance companies follow to adhere to standards and regulations governing the healthcare industry. This feature helps with maintenance of precise documentation, protecting user information and following the coding procedures as required by the law.
3. Automated Adjudication
A healthcare claim management application should be capable of automating the adjudication process. The automation involves accurate and efficient evaluation of claims based on a predefined set of rules, minimizing the need for manual intervention. This also minimizes the processing time.
4. Denial Management
A claim management tool can help minimize the denial rates by identifying and analyzing the common reasons for denials. It helps insurers and service providers address those reasons in advance and implement preventive measures to minimize the chances of future denials.
5. Eligibility verification
It is important for healthcare providers to verify the eligibility of patients for insurance claims to minimize frauds and false claims. So, service providers and insurers should ensure that the software they consider using has the feature to verify the eligibility of patients for claims, ensuring precision and minimization of denials.
6. Third Party Access
Healthcare claims involve the intervention of several parties including healthcare providers, insurers or third parties to which they outsource processes like documentation, user verification or data collection. Therefore, a medical claim management tool should have the feature to allow access to third parties for faster processing of claims.
7. Customer Support
Due to the detailed features involved in the claim management software, users need support from experts while using it. Whether a claim management software is being used by healthcare providers, insurance companies, patients or third parties, it should come with customer support.
Additional Features To Consider That Put You Above the Rest
You’re smart enough to realize that the right features can elevate your system, improve efficiency, and enhance the user experience for both providers and patients. Here are a few additional capabilities that can set your claims management process apart from the rest.
1. Multi-Device Access
Most users use multiple devices, such as laptops, tablet PCs, and smartphone,s which may have different operating systems. A software that comes with mobile apps and versions for various devices such as Android, windows, and iOS can be accessed by users on multiple devices.
2. Payments Integration
The ability to integrate payments in the claims management software or application enables healthcare providers and insurers to recover overpayments from end users. It also allows patients to make payments to insurers and healthcare providers.
3. Integration with Other Apps
A claims management software or application with integration capabilities allows users to integrate it with health insurance apps, payment apps and health care providers apps. This allows faster tracking, data processing and user satisfaction.
How to Choose the Right Healthcare Claim Management Tool?

Considering the importance and benefits of claims management software ensures that it is a must-have tool not only for service providers and insurers but also for patients and third parties. However, it is crucial to choose the right claim management software to ensure it satisfies users' requirements and helps with the smooth functioning of insurers and faster processing of claims. Here are some factors you should consider while choosing a healthcare claim management solution for your business.
1. Functionality
There are a variety of claims management software available that cater to a variety of industries. The software should offer specific features for the healthcare industry and support the types of healthcare claims. Users should consider choosing software specially designed for healthcare claims.
2. Integration
Users should ensure that the software or application comes with integration capabilities. The application should be integrable with your existing systems and applications, such as CRM, accounting, or medical billing software.
3. User Interface
Consider a custom healthcare software solution that comes with an easy-to-use interface that your staff can understand and navigate easily. If you prefer customization, consider choosing an application that offers user customization features.
4. Cost
It is important to evaluate the price of the healthcare claims management application. The price should include customization costs, user support, and updates. The software should offer a good ROI for your business.
5. Customer Support
Users often need support at various stages of healthcare claim management. Consider a software provider that offers dedicated customer support, including technical assistance and resolution of health insurance issues.
6. Security
When it comes to handling of user data, security is a crucial factor to consider. Look for a claim management tool that offers high levels of data protection measures, such as multifactor authentication and end-to-end encryption.
Streamline Your Claims Management Process Effortlessly & Efficiently With AI!
At DITS, We empower you to Automate billing workflows, reduce denials, and enhance operational efficiency with cutting-edge healthcare claims software.
Role of AI In Healthcare Claims Management Software
As we look to the future, healthcare claims management is evolving rapidly, with technology at the helm. Key trends are shaping the way claims are processed, improving speed, efficiency, and user satisfaction. Here's a look at what’s on the horizon:
1. AI-Driven Automation
Automation powered by AI is transforming healthcare claims. From faster claims processing to real-time eligibility verification, AI will handle tedious tasks, significantly reducing human error and expediting claim approvals. With machine learning algorithms constantly learning from data, these systems will become smarter over time.
2. Advanced Data Analytics for Smarter Decision-Making
Data analytics will play a pivotal role in the future of claims management. With the ability to analyze large datasets in real time, healthcare providers and insurers can identify trends, detect anomalies, and make more informed decisions. This empowers them to address potential issues before they even arise, ensuring smoother claim processing.
3. Enhanced User Experience Through Personalization
As technology evolves, so will the user experience. Healthcare claims management systems will use data to provide a more personalized approach for each user. Whether it's tailored communication or customized workflows, these advancements will result in smoother, more intuitive interactions.
4. Integration of IoT for Real-Time Data Access
The Internet of Things (IoT) will have a significant impact on healthcare claims management by integrating real-time data from wearable devices and other healthcare tools. This will allow insurers to track patient conditions, validate claims with immediate data, and speed up the process, creating a more seamless experience for all parties.
5. Streamlined Third-Party Integrations
Healthcare claims management systems will become more interconnected with third-party platforms, such as electronic health record (EHR) systems, payment apps, and other healthcare management tools. These integrations will ensure faster, more accurate data exchanges, reducing delays and errors in the claims process.
Let DITS Help You With Premier Custom Healthcare Software Solutions!
At DITS, we are already ahead of the curve in incorporating these technologies into our healthcare claims management solutions. Our expertise in developing customized, innovative software allows us to provide solutions that not only meet current needs but also anticipate future demands.
Want to future-proof your healthcare claims management process?
Contact DITS today to discover how our cutting-edge solutions can streamline your operations, enhance security, and improve the overall user experience.
FAQs
1. What is medical claim management?
Medical claim management is the step-by-step process of handling healthcare claims submitted by patients or healthcare service providers. It includes submission, processing and managing the claims between service providers, medical insurance companies and patients. These claims are requests submitted by patients or healthcare providers for reimbursement of costs for medical services.
2. Why is medical claim management important?
Medical claims management is essential to ensure that healthcare providers receive the payments for the services offered to patients. It also helps patients to utilize and take maximum benefit from their health insurance plan. In addition, claim management services help insurers with a smooth and efficient processing of medical claims.
3. What are the most common features of healthcare claim management software?
Claim tracking, eligibility verification, compliance management, automated adjudication, denial management, data security, and customer support are some key features that users must consider while choosing healthcare claim management software.
Users may also consider some additional features like multiple device access, payment facilities, and integration with other applications.
4. Why should you consider developing custom healthcare claim management software?
Standard healthcare claims software may lack the features you want for your organization. Software with limited customization may offer irrelevant features, lack of scalability, compliance and compatibility issues.
Also, it may offer limited control and flexibility while working on medical claims. However, customizable software is tailored to your unique needs and offers greater control and flexibility over customization. You can modify the system as required without relying on third parties.
5. How does medical claim management software reduce operational expenses?
A medical claims software automates certain processes such as document handling, data analysis, decision-making and claim settlements. Automating the claim management processes also reduces administrative overhead and minimizes fraudulent claims. Automating such tasks minimizes the need for human intervention, which in turn saves costs and resources.
6. How much does it cost to develop healthcare claim management software?
The cost to develop a healthcare claim management solution depends on several factors, such as features, complexity, technology stack, third-party integrations, maintenance and support. However, we can offer you a rough estimate of the cost with these points.
A basic claim management software usually costs from $50k to $150k. A mid-range solution can cost between $150k and $500k. However, enterprise-level claim management software may cost more than $500K.

Nidhi Thakur
With more than 19 years of experience - I represent a team of professionals that specializes in the healthcare and business and workflow automation domains. The team consists of experienced full-stack developers supported by senior system analysts who have developed multiple bespoke applications for Healthcare, Business Automation, Retail, IOT, Ed-tech domains for startups and Enterprise Level clients.
Recent Posts

Discover AI techniques used in chatbots like NLP, machine learning, and intent recognition that help businesses automate conversations, improve accuracy, and enhance customer engagement.

Let's explore top 10 uses of Artificial Intelligence in Mental Health and how it is transforming lives and enhancing patient outcomes across a range of mental health conditions.

Facial recognition software costs range from $5,000 to $500,000+, depending on features, deployment type, accuracy, and compliance requirements.